Why are DHEA & Testosterone Important?
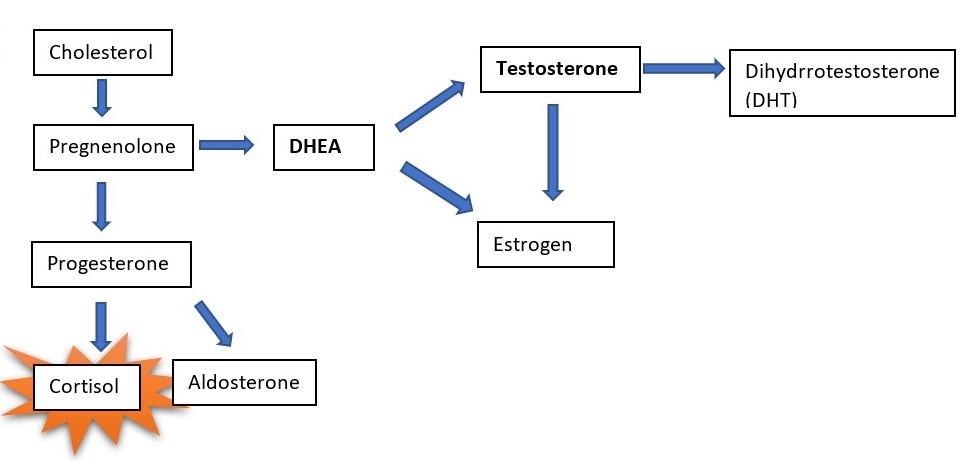
Testosterone is a male hormone, right? True, but females need it just as much as males do, just in smaller amounts. Not only is necessary for a healthy libido and sexual satisfaction, but it is also essential for bone health, brain health, muscle health, and heart health. It needs to be in balance with the other female hormones, estrogen, and progesterone (sex steroids), thyroid hormones, as well as our major stress hormone, cortisol, in order to function optimally. The Androgen DHEA is a feel-good hormone. It gives one a feeling of well being, libido, good sleep, muscle strength, and exercise tolerance.
What are the common symptoms of DHEA deficiency?
Common symptoms of DHEA deficiency include reduced sex drive, reduced sexual sensitivity, difficulty achieving orgasm, painful intercourse, low mood and excessive anxiety, poor coping ability, reduced muscle tone and strength, joint pain, back pain, dry skin, poor memory or concentration and urinary incontinence. The symptoms can overlap with hormonal and other medical conditions. Thus, androgen deficiency often goes under-diagnosed and is not often thought to be relevant in females.
Cortisol Steal
So where does it all go wrong and why are we seeing so many women, young and old, with deficiency these days? Cortisol steal. This is exactly what it sounds like. Cortisol is stealing the substrates that our sex steroids and DHEA need to be formed because it is being produced in excess. DHEA becomes depleted and because this is upstream from testosterone (and estrogen), these downstream hormones also become depleted. So it’s the stressed women that get more hormonal issues. It is not the hormones’ fault. They are just responding appropriately to other imbalances in the body. Why would you need to reproduce or have sex for that matter, if you are running away from a lion?
Stress and Hormones
The body interprets internal and external stress as the same thing. It doesn’t know the difference between having a fight with someone vs candida overgrowth in the gut, for example. It responds by releasing cortisol and other stress hormones and neurotransmitters from the adrenal glands. When cortisol is produced in excess, the hypothalamus in the brain perceives a threat. It switches off signals to the adrenals and cortisol is no longer produced. Alongside this, high cortisol triggers DHEA release, which tries to balance the high cortisol. With DHEA and cortisol levels low, the patient experiences stage 3 adrenal fatigue. The new term for this is HPA axis dysfunction/ dysregulation.
Replacing DHEA and Testosterone in Women
DHEA and testosterone can be replaced alone, or alongside each other in women. It should be ensured that the other female hormones are also optimal. In our practice, we prescribe bioidentical hormones, which are hormones that behave in an exact way as our own hormones. They are still laboratory-made but are chemically identical to our hormones. The bad rap that hormone replacement has is from synthetic hormones, which confuse our hormonal systems – like putting the wrong key into a lock. Testosterone is most often prescribed topically, or in certain cases intramuscularly/ subcutaneous. DHEA is most often prescribed sublingually or by mouth, but can also be given topically.
The key to safe hormone replacement is testing your levels (24 hour urine hormone is the best test for this, but blood levels can be used when resources are limited). Once on the treatment, levels should be monitored by an experienced health care professional in order to find the dose that is right for you. This can vary tremendously between women, depending on genetics, underlying factors that caused the hormone deficit and lifestyle (a very active woman requires more DHEA or testosterone, often). You can find your optimum dose by looking at your levels alongside your symptoms.
What else can you do to improve your levels besides taking hormones?
Hormone replacement is not the only answer but in every case, should be done alongside root cause treatment and lifestyle changes. Hormone replacement does not fix the adrenals and other hormones. It is just another patch if done alone. Some women even feel worse on hormones, which tells us we need to work on these root causes.
Other Lifestyle Improvements
So what can you do to help these hormones in your day to day life? Your overall aim is to decrease inflammation and stress on the HPA axis.
Diet
An anti-inflammatory diet is a good place to start. Many hormone disturbances start in the gut, because of a constant onslaught of foods that increase inflammation, upregulate our immune system, change our microbiome, and impact our gut-brain connection. Sugar, carbohydrates, and dairy are big contributors to poor hormone health.
Exercise
Make sure you are getting exercise that is appropriate for your condition. Don’t run a marathon when your adrenals are shot.
Sleep
Make sure you get at least 7-8 hours of sleep each night. Good sleep hygiene is essential and your health care professional may recommend supplements and medications for this.
Stress Management
Make sure you are identifying and managing stress – we cannot always change our stressful circumstances but we can change how we perceive them and what we do every day to find our calm.
We recommend 2 books to find out more: The Hormone Handbook by Dr. Thierry Hertoghe; and, What You Must Know About Women’s Hormones: Your Guide to Natural Hormone Treatments for PMS, Menopause, Osteoporis, PCOS, and More by Dr. Pamela Wartian Smith.
About the author:
One of Dr. Michelle’s greatest passions in life is to help people help themselves. She understands that your current health tells a story and that when you have symptoms of disease, your body is already out of balance. She believes that we should not have to settle for anything other than our most vital self and that her job is to figure out how to put you back on track. To book an appointment with Dr. Michelle, contact [email protected]